GMP’s for Early Stage Development of New Drug substances and products
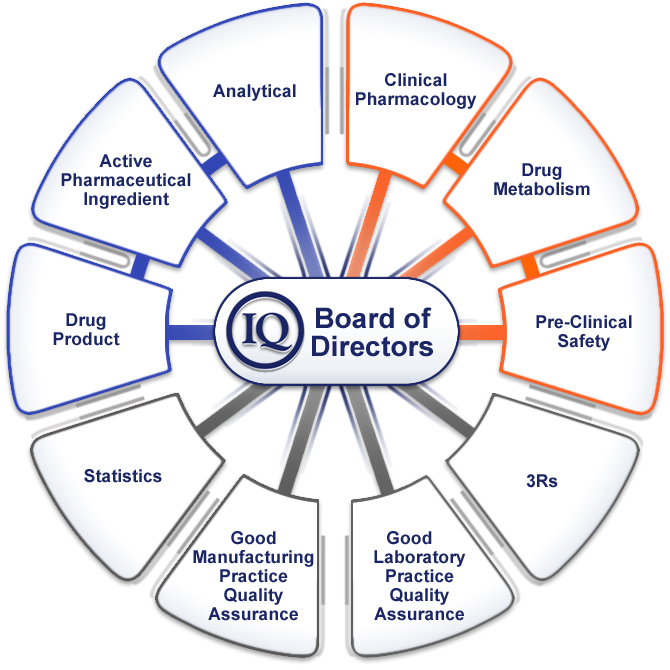
The question of how Good Manufacturing Practice (GMP) guidelines should be applied during early stages of development continues to be discussed across the industry and is now the subject of a new initiative by the International Consortium on Innovation and Quality in Pharmaceutical Development (IQ Consortium)—an association of pharmaceutical and biotechnology companies aiming to advance innovation and quality in the development of pharmaceuticals. They have assembled a multidisciplinary team (GMPs in Early Development Working Group) to explore and define common industry approaches and to come up with suggestions for a harmonized approach. Their initial thoughts and conclusions are summarized in Pharm. Technol. 2012, 36 (6), 54–58.
From an industry perspective, it is common to consider the “early” phase of development as covering phases 1 and 2a clinical studies. During this phase, there is a high rate of product attrition and a high probability for intentionally introducing change into synthetic processes, dosage forms, analytical methods, and specifications. The quality system implemented during this early phase should take into account that these changes and adjustments are intrinsic to the work being performed prior to the determination of the final process and validation of the analytical methods during later stages of development.
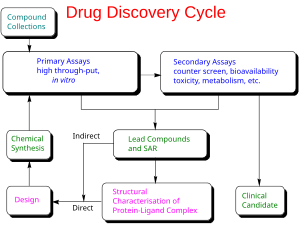
FDA guidance is already available on GMP requirements for phase 1 materials. (See Org. Process. Res. Dev. 2008, 12, 817.) Because many aspects of phase 2a clinical studies are similar in their scope and expectations, the working group feels there is an opportunity to extend this guidance across all early phase studies. Because products and processes are less well understood in the early phases of development, activities should focus on accumulating the appropriate knowledge to adequately ensure patient safety. Focusing on this area should ensure that beneficial therapies reach the clinic in an optimum time scale with minimal safety concerns.

A follow-up article ( Pharm. Technol. 2012, 36 (7), 76−84) describes the working group’s approach to the subject of Analytical Method Validation. Their assessment has uncovered the need to differentiate the terms “validation” and “qualification”. Method qualification is based on the type, intended purpose, and scientific understanding of the type of method in use. Although not used for GMP release of clinical materials, qualified methods are reliable experimental methods that may be used for characterization work such as reference standards and the scientific prediction of shelf life. For example, in early development it would be sufficient for methods used for in-process testing to be qualified, whereas those methods used for release testing and for stability determination would be more fully validated.
In early development, a major purpose of analytical methods is to determine the potency of APIs and drug products to ensure that the correct dose is delivered in the clinic. Methods should also indicate stability, identify impurities and degradants, and allow characterization of key attributes. In the later stages, when processes are locked and need to be transferred to worldwide manufacturing facilities, methods need to be cost-effective, operationally viable, and suitably robust such that the methods will perform consistently. irrespective of where they are executed.
The authors advocate that the same amount of rigorous and extensive method-validation experiments, as described in ICH Q2, “Analytical Validation”, is not needed for methods used to support early stage drug development. For example, parameters involving interlaboratory studies (i.e., intermediate precision, reproducibility, and robustness) are not typically performed during early phase development, being replaced by appropriate method-transfer assessments and verified by system suitability requirements. Because of changes in synthetic routes and formulations, the impurities and degradation products formed may change during development.
Accordingly, related substances are often determined using area percentage by assuming that the relative response factors are similar to that of the API. As a result, extensive studies to demonstrate mass balance are typically not conducted during early development.
Detailed recommendations are provided for each aspect of method validation (specificity, accuracy, precision, limit of detection, limit of quantitation, linearity, range, robustness) according to the nature of the test (identification, assay, impurity, physical tests) for both early- and late phase development. These recommendations are also neatly summarized in a matrix form.
Above text drew attention to a series of articles from the IQ Consortium (International Consortium on Innovation and Quality in Pharmaceutical Development) on appropriate good manufacturing practices (GMP) for the early development phases of new drug substances and products. The fifth article in this series(Coutant, M.; Ge, Z.; McElvain, J. S.; Miller, S. A.; O’Connor, D.; Swanek, F.; Szulc, M.; Trone, M. D.; Wong-Moon, K.; Yazdanian, M.; Yehl, P.; Zhang, S.Early Development GMPs for Small-Molecule Specifications: An Industry Perspective (Part V) Pharm. Technol. 2012, 36 ( 10) 86– 94) focuses on the setting of specifications during these early phases (I and IIa).
Due to the high attrition rate in early development, the focus should be on consistent specifications that ensure patient safety, supported by preclinical and early clinical safety studies. On the basis of the cumulative industry experience of the IQ working group members, the authors of this paper propose standardized early phase specification tests and acceptance criteria for both drug substance and drug product. In addition to release and stability tests, consideration is given to internal tests and acceptance criteria that are not normally part of formal specifications, but which may be performed to collect information for product and process understanding or to provide greater control.
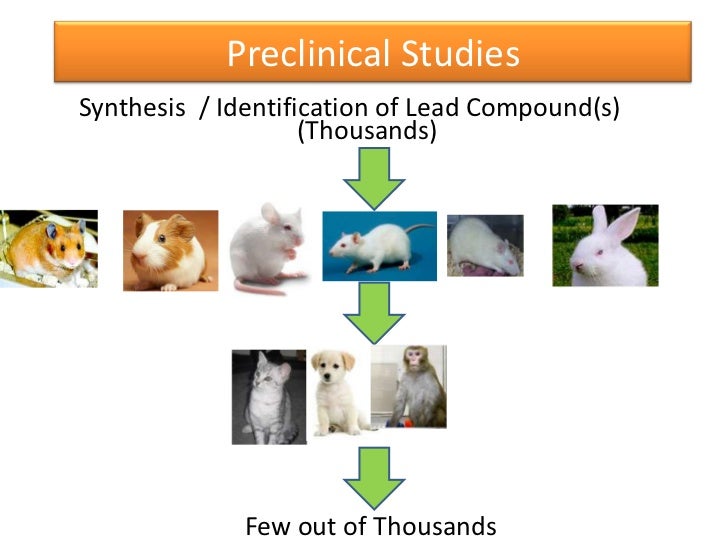
The drug substance used in preclinical animal studies (tox batch) is fundamental in defining the specifications for an early phase clinical drug substance (DS). Here, internal targets rather than formal specifications are routinely used while gathering knowledge about impurities and processing capabilities. At this stage the emphasis should be on ensuring the correct DS is administered, determining the correct potency value, and quantitating impurities for toxicology purposes. For DS intended for clinical studies, additional testing and controls may be required; the testing may be similar to that for the tox batch, but now with established acceptance criteria. For these stages the authors propose a standardized set of DS specifications, as follows.
| Description | range of colour |
| identification | conforms to a reference spectrum |
| counterion | report results |
| assay | 97–103% on a dry basis |
| impurities | NMT 3.0% total, NMT 1.0% each |
| unidentified | NMT 0.3% |
| unqualified | NMT 0.15% |
| mutagenic | follow EMA guidelines (pending ICH M7 guidance) |
| inorganic | follow EMA guidelines (pending ICH Q3D guidance) |
| residual solvents | use ICH Q3C limits or other justified limits for solvents used in final synthetic step |
| water content | report results |
| solid form | report results |
| particle size | report results |
| residue on ignition | NMT 1.0% |
These may be altered in line with any specific knowledge of the compound in question. For example, if the DS is a hydrate or is known to be hygroscopic or sensitive to water, a specified water content may be appropriate. Of particular note is the use of impurity thresholds which are 3 times higher than those defined in ICH Q3 guidelines. Q3 was never intended to apply to clinical drugs, and higher thresholds can be justified by the limited exposure that patients experience during these early stages. Mutagenic impurities are the exception here, since in this area the existing official guidance does cover clinical drugs.
The fourth article in the series(Acken, B.; Alasandro, M.; Colgan, S.; Curry, P.; Diana, F.; Li, Q. C.; Li, Z. J.; Mazzeo, T.; Rignall, A.; Tan, Z. J.; Timpano, R.Early Development GMPs for Stability (Part IV) Pharm. Technol. 2012, 36 ( 9) 64– 70) considers appropriate approaches to stability testing during early clinical phases. Appropriate stability data at suitable storage conditions are required to support filing the clinical trial application (CTA/IND/IMPD) and use of the clinical material through the end of the clinical study. Several factors from business, regulatory, and scientific perspectives need to be taken into account when designing early stability studies, such as the risk tolerance of the sponsoring organization, the inherent stability of the drug substance and prior product, process and stability knowledge, the regulatory environment in the countries where the clinical trial will be conducted, and the projected future use of the product.
Often non-GMP DS batches are manufactured first and placed on stability to support a variety of product development activities.In many cases these batches will be representative of subsequent GMP batches from a stability perspective and can be used to establish an initial retest period for the DS and support a clinical submission. In early development, it is common for the manufacturing process to be improved; therefore, as the DS process evolves, an evaluation is needed to determine whether the initial batch placed on stability is still representative of the improved process. The authors advocate a science- and risk-based approach for deciding whether stability studies on new process batches are warranted.
The first step is to determine which DS attributes have an effect on stability. This step can be completed through paper-based risk assessments, prior knowledge, or through a head-to-head short-term stability challenge. If the revised process impacts one or more of these stability-related quality attributes, the new batch should be placed on stability—otherwise not. Typical changes encountered at this stage include changes in synthetic pathway, batch scale, manufacturing equipment or site, reagents, source materials, solvents used, and crystallization steps.

In most cases, these changes will not result in changes in DS stability. Changes to the impurity profile are unlikely to affect stability, since most organically related impurities will be inert. On the other hand, catalytic metals, acidic or basic inorganic impurities, or significant amounts of residual water or solvents may affect stability; thus, changes to these attributes would typically require the new batch to be placed in the stability program. Similarly, any changes to polymorphic form, particle size, or counterion would warrant extra testing. Packaging changes of the bulk material to a less protective package may require stability data to support the change.
Three approaches to stability data collection are commonly used. One is that an early, representative DS batch is placed under real-time and accelerated conditions (e.g., 25 °C/60% RH and 40 °C/75% RH), and stability results for a few time points (e.g., 1–6 months) are generated to support an initial retest period (e.g., 12 months or more). A second approach is to use high stress conditions such as a high temperature and high humidity with a short time. A third approach is the use of stress studies at several conditions coupled with modelling. The retest period derived from these types of accelerated or stress studies can be later verified by placing the first clinical batch into real-time stability studies under ICH accelerated and long-term conditions. Future extensions of the retest/use period can be based on real-time data.

Ref
“ALL FOR DRUGS” CATERS TO EDUCATION GLOBALLY, No commercial exploits are done or advertisements added by me. This article is a compilation for educational purposes only.
P.S. : The views expressed are my personal and in no-way suggest the views of the professional body or the company that I represent
////////












